LIE: "The difference between cancer and non-cancer pain is an evidence-based distinction and one that's easy to determine. Cancer pain has adequate pain treatment."
One thing that most opioid prescribing guidelines have in common is they categorize pain into cancer vs non-cancer. At a glance, that distinction makes sense, right? But is it an evidence-based difference? Or, are policies once again being created based on arbitrary distinctions that are actually meaningless? We break it all down for you in this article. We show you the origin of the distinction, petitions where the distinction was requested, meetings where it was discussed, and guidelines where it was used. We also discuss whether actual cancer pain is being treated adequately.
This article contains the following information:
- Where is the cancer vs. non-cancer pain distinction being made?
- Who asked for the distinction to be included in labels and guidelines?
- Did the FDA take PROP's petition seriously?
- What was FDA's written response to PROP regarding their petition?
- What's the origin of the distinction between cancer vs non-cancer pain and is it based on science?
- Should "cancer pain" receive opioids?
- Does "cancer pain" get adequate pain treatment?
- Is there stigma involved with "cancer pain" and opioids?
- Are there studies showing benefits of using opioids in terminal cancer patients?
- Summary
Where Is the Cancer Vs. Non-Cancer Distinction Being Made?
Let's start with some opioid prescribing guidelines. The 2007 AMDG (Washington State Medical Director's Group Interagency Guidelines) are called "Interagency Guideline on Opioid Dosing for Chronic Non-cancer Pain." The 2016 CDC Guidelines state in the summary "This guideline provides recommendations for primary care clinicians who are prescribing opioids for chronic pain outside of active cancer treatment, palliative care, and end-of-life care." The updated/expanded CDC Guidelines are due to come out the end of 2022. At the very top of the Opioid Workgroup (OWG) report, they state "this document outlines the observations of the Opioid Workgroup on the updated CDC Guideline for Prescribing Opioids. CDC recommendations for prescribing opioids for outpatients with pain outside of sickle cell disease-related pain management, cancer pain treatment, palliative care, and end-of-life care." We actually weren't able to find any opioid guidelines that didn't make this distinction.
Who Asked For the Distinction To Be Included in Labels and Guidelines?
On July 25, 2012, PROP (Health Professionals for Responsible Opioid Prescribing), led by the then president, Andrew Kolodny, sent the FDA a citizen's petition. The petition had over 35 signatures including would be expert witnesses in opioid litigation such as Anna Lembke and Jane Ballantyne. Soon to be author of both the 2016 and 2022 CDC Guidelines, Roger Chou, also signed it. The purpose of the petition was to ask the FDA to change their labeling of prescription opioids. The following requests were made:
1. Strike the term “moderate” from the indication for non-cancer pain.
2. Add a maximum daily dose, equivalent to 100 milligrams of morphine for non-cancer pain.
3. Add a maximum duration of 90-days for continuous (daily) use for non-cancer pain.
As you can see, the concept of pain being put in two groups of cancer vs non-cancer was central to each request in PROP's petition to the FDA.
Did the FDA Take PROP's Petition Seriously?
It is unclear how this one citizen's petition had so much power, but it did. Let's look at some of the discussions that took place due to the petition.
MEETING #1: In May of 2012 the NIH sponsored a meeting with the FDA called "Assessment of analgesic treatment of chronic pain: a scientific workshop." Read through the transcripts for these all- day meetings held on May 30 and May 31, 2012. You can browse the public comments here. This meeting was not specifically supposed to be about opioid labels and PROP's requests, but looking through the transcripts of both days, this request to change the opioid labeling seemed to be the main topic of conversation. People like Kolodny, Ballantyne, Rummler all spoke at this meeting, basically demanding the change in opioid labels. FDA pushed back repeatedly claiming there wasn't enough evidence to make such a drastic change. As they stated in the meeting, a main goal of this change in label would be to restrict access to pain medication for patients. So even if a doctor would prescribe opioids "off-label," insurance would refuse it.
MEETING #2: In February of 2013, the FDA held a two-day meeting to address the concerns and requests of PROP's citizen's petition. The meeting was called "Impact of approved drug labeling on chronic opioid therapy. Part 15 public hearing" and was held on Feb 7 and Feb 8, 2013. You can browse some of the 1900 comments that were submitted here. There are some comments from people or organizations that supported PROP's requests, but the vast majority didn't agree with their petition. Here is a quote from one of the comments submitted by American Society of Anesthesiologists (ASA ) "A fundamental flaw shared by all three components of the PROP proposal is the intrinsic difficulty in defining “non-cancer pain.” Improvements in cancer therapy have resulted in increases in survival duration as well as cure rates, although the treatments used to achieve these beneficial results often lead to chronic pain. Who will decide whether the persistent pain, for example, of herpes zoster or nerve damage incurred during an otherwise curative course of chemo- and radiation therapy is or is not cancer-related?"
Dr. Bob Twillman, a pain psychologist, spoke at the meeting on February 7. He said "I think creating indications based on whether the cause of pain originates with cancer or not is inappropriate. I think one wrong question is, should we use opioids to treat chronic non-cancer pain? I think an alternative which may be one of the right questions is, in which patients should we use opioids to treat chronic non-cancer pain? at what doses? for how long? with which precautions?" He then goes on ask about this distinction stating similar concerns as the ASA made in their docket comment. At what point does cancer pain become non-cancer pain? Is it upon waking up from surgery to remove cancer? Is it once the patient is in remission?
Dennis Capolongo from the Arachnoiditis Society for Awareness and Prevention (ASAP) said "In a recent letter from PROP to our director, Dr. Kolodny admits that the model for his petition was flawed, since it failed to consider incurable, non-cancerous disorders, such as arachnoiditis. Therefore we wish to propose that a third category be created for these incurable, non-cancerous conditions, one that would recognize, first recognize the severity of the modality and then it exempts sufferers from any restrictive policies that would limit their access to opioid consumption, since there's no other treatment."
Here is another quote by a presenter at this meeting: "So one of the questions that you've asked of us requests the methods used for distinguishing cancer and non-cancer pain. That's the big theme here. And the short answer from the American Cancer Society is that we don't draw any such line in policy or practice. The opioid receptors, they don't know or care if someone has cancer. Nor do those receptors respond only when someone is nearing the end of life."
What Was FDA's Written Response to PROP Regarding Their Petition?
After these workshops were held and public comments received, the FDA sent PROP a response to their citizen's petition. The response addressed all of PROP's requests. For this article, we will just focus on the part of the letter that involved the cancer vs. non-cancer distinction.
"All of PROP's labeling change requests are linked to "non-cancer" pain, a distinction that is not made in current analgesic labeling. It is FDA's view that a patient without cancer, like a patient with cancer, may suffer from chronic pain, and PROP has not provided scientific support for why labeling should recommend different treatment for such patients. In addition FDA knows of no physiological or pharmacological basis upon which to differentiate the treatment of chronic pain in a cancer setting or patient from the treatment of chronic pain in the absence of cancer, and comments to the petition docket reflect similar concerns. FDA therefore declines to make a distinction between cancer and non-cancer chronic pain in opioid labeling."
So there isn't any evidence supporting this distinction. That didn't stop it from making its way into guidelines and laws based on guidelines.
What's The Origin Of the Distinction Of Cancer Vs Non-Cancer Pain and Is It Based On Science?
In an article on March 3, 2016 called "Chronic Cancer versus Non-Cancer Pain: A Distinction without a Difference?" the author discusses arguments that were used in political debates. He calls one of these fallacies the “sham distinction,” which is now known better as a 'distinction without a difference." "This logical fallacy appeals to a distinction between two two things that ultimately cannot be explained or defended in a meaningful way. When it comes to cancer and non-cancer pain, one really must question why we are drawing a distinction between these two entities and whether it is science or politics that that demands there be a difference."
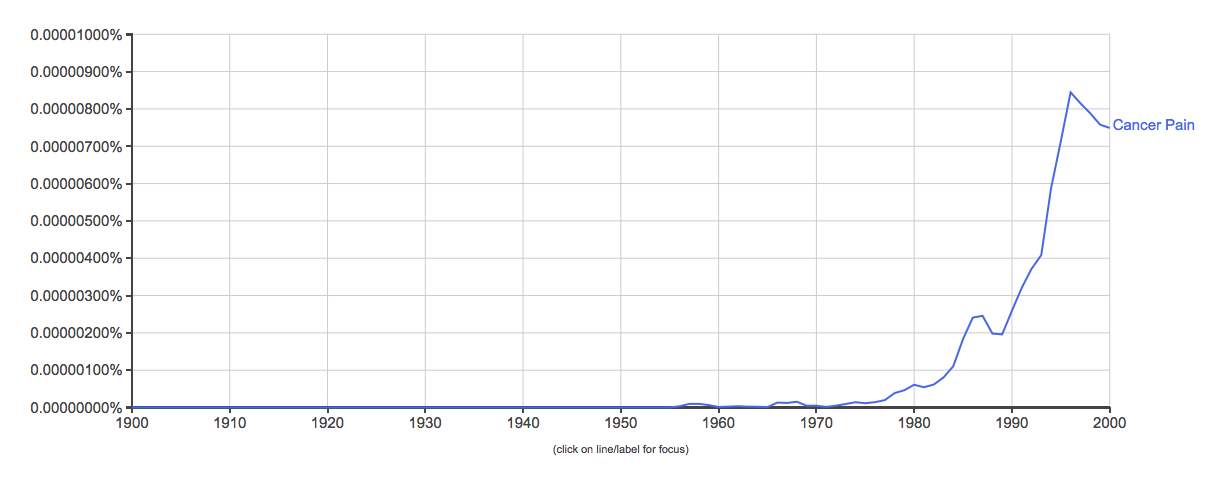
According to this graph in the article, the terms cancer pain and non-cancer pain are relatively new, really taking off in the past few decades in medical literature.
An article by Schatman and Peppin in 2016 called "Terminology of Chronic Pain, the need to level the playing field," states "“Chronic cancer pain” and “chronic non-cancer pain” are replete in the literature; however, the distinction here is actually obscure. A patient with pain from a cancer etiology has no different physiology than a patient with pain of non-cancer etiologies." The authors go on to describe the origin of the distinction as a "move in the 1990's to change the way chronic pain in patients without cancer was treated." Agreeing with the point others made that there isn't evidence of a true difference between the two types of pain, the authors suggest insisting on a difference between the two can be interpreted in the following ways:
-
"We do not care if the patient with cancer suffers from side effects, fatal or otherwise from opioids, and/or develops a substance-use disorder. But we do care if a patient with chronic “noncancer” pain develops these problems."
-
"We do not care if patients with noncancer pain suffer; they are not “worth” the effort of adding opioids to their regimens."
Schatman and Peppin state the purpose of their article isn't to say whether someone with cancer or without cancer should be given opioids, but that it should be acknowledged that the basis for this distinction isn't scientific evidence. They "suggest that the terminology be changed to help us better to understand and treat all of our chronic pain patients who are suffering. Categorization into “cancer” and “non-cancer” does not help us better understand mechanisms underlying pain or guide us to appropriate treatment strategies. Further, these categories are philosophical and neither scientific nor of clinical relevance" "The goal here is to continue to be patient-focused, relieve their suffering (instead of contributing to it), and help improve their lives. Language, in and by itself, is obviously not a “cure” for pain. However, clinicians and society as a whole need to appreciate language’s potential to further stigmatize and marginalize all patients suffering from chronic pain, and accordingly we are obliged to work toward a more language-neutral system of pain classification."
In the article, the author states "From a medical and scientific aspect, it makes little sense to have these two broad categories of chronic pain. But from a political and emotional aspect, it may make ones life a little easier, because who doesn’t want to relieve the pain of a dying cancer patient. But what about a cancer survivor? Are they still considered to have cancer pain once the cancer is cured? What if the pain is due to chemotherapy-induced neuropathy? Who will fight their battle politically?"
"While it may feel wise to distinguish the terms cancer and non-cancer pain from each other, continued promotion of this idea is fraught with logical fallacies, and is best defended by emotions and politics rather than the state of science. The alternative is to abandon the distinction for all of these reasons and use terms that actually help us understand the nature of an individuals pain and how best to manage it, which may or may not include opioids."
We've shown you several articles explaining how the distinction between cancer and non-cancer pain is nonsensical. We've shown you PROP's request for this distinction to be made, and the workshops that were held to discuss this distinction. We've shown FDA's response to PROP explaining how they neglected to show that this distinction is evidence-based.
AND YET.... it continues to be used in opioid prescribing guidelines and state laws based on these guidelines. We've also seen it make its way into indictments against doctors.
"Should "Cancer Pain" Receive Opioids?
Just for fun, let's pretend there is a clear delineation between cancer and non-cancer pain. Considering this distinction has become common practice, you'd think there is some consensus as to how "cancer pain" should be treated. Sadly, there isn't. We found many articles and presentations from "experts" discussing the idea of not using opioids for cancer pain. I don't have a problem with multi-modal cancer pain treatment. What I do object to is the entire goal of any treatment being "let's use anything and everything except for opioids."
Here is one example of a presentation about not using opioids for breast cancer patients.
"Alternatives to Opioids for Breast Cancer Pain."
Notice the speaker gives a shout out to Andrew Kolodny, and then immediately quotes a false statistic that "80% of heroin users started with a prescription from their doctor." We've debunked this lie in detail here. The WHO (World Health Organization) has created a step ladder for the treatment of cancer pain. This presentation from Maimonides Hospital in Brooklyn, NY seems to contradict WHO.
Here is another presentation called "Treating Cancer Pain Without Opioids." This one seems a bit more balanced and acknowledges that opioids can and should be used in cancer pain.
Does "Cancer-Pain" Get Adequate Pain Treatment?
Now that we've shown that guidelines continue to make this distinction of cancer vs non-cancer pain, let's talk about what that actually means for the cancer pain sufferer? Is it truly the holy grail of all painful illnesses that is given adequate opioids when needed? Well, I used to think it was. Until we started to get calls from cancer patients who were being denied opioids. Here is a video of a terminal cancer patient, April, who was denied opioids at the pharmacy. April has since passed away. We are grateful she told her story so people know what's happening even to those with "cancer pain."
- In this article "The downgrading of pain sufferers' credibility," a study was discussed that was conducted by the US Department of Health and Human Services that revealed that “more than 50 percent of cancer patients didn’t receive adequate analgesia, and about 25 percent of them were estimated to die in severe, unrelieved pain.” That should be appalling to read. Yet, we found many articles and presentations discussing the fact that there is over prescribing of opioids even in "cancer pain," and how it needs to stop.
- In the article "US Trends in Opioid Access Among Patients With Poor Prognosis Caner Near the End-of-Life," the author concludes that "Opioid use among patients dying of cancer has declined substantially from 2007 to 2017. Rising pain-related ED visits suggests that end-of-life cancer pain management may be worsening."
Is There Stigma Involved With Cancer Pain And Opioids?
- In this article called "Oncologists' Views on Challenges in Opioid Prescribing for Patients with Cancer-related Pain," the author lists the following challenges in prescribing opioids for cancer-related pain:
- Patients who receive opioids feel stigmatized by clinicians, pharmacists, and society.
- Patients fear becoming addicted, affecting their willingness to accept prescription opioids.
- Guidelines for safe and effective opioid prescribing are often misinterpreted, leading to access issues.
- In this article called "Are Cancer Patients Getting the Opioids They Need to Control Pain," the authors "suggested, measures to make opioids harder to obtain may have prevented some patients from receiving appropriate prescriptions for opioids to manage cancer pain." They also stated “It appears that oncologists are not prescribing opioids as much as they did previously and that "future research needs to focus on whether opioid prescribing guidelines intended for patients without cancer are being applied inappropriately to patients who have had cancer.”
Are There Studies Showing Benefits Of Using Opioids In Terminal Cancer Patients?
- A recent study came out called "Opioid Use Linked to Survival in Older Patients With Advanced Pancreatic Cancer." It concluded that "opioid prescriptions are associated with increased survival in elderly patients with advanced disease suggests that symptom mitigation should be emphasized in clinical treatment of pancreatic cancer."
So, once again, we've shown that the basis of these "evidence-based" guidelines are truly opinion based. There is no way to distinguish the two types of pain. When does it switch from cancer pain to non- cancer pain? Is it upon waking up from cancer removal surgery? What about chronic pain the patient has that is unrelated to their actual tumor? Is that non-cancer pain since the cause isn't cancer? We used to think cancer was the "holy grail" of painful conditions that would allow adequate pain treatment. Sadly, non even "cancer-pain" will guarantee that someone will receive needed opioids. Once again quoting Schatman and Peppin, for those who insist on placing all pain into the two categories of cancer and non-cancer, which of the following statements are they actually saying?
-
"We do not care if the patient with cancer suffers from side effects, fatal or otherwise from opioids, and/or develops a substance-use disorder. But we do care if a patient with chronic “noncancer” pain develops these problems."
-
"We do not care if patients with noncancer pain suffer; they are not “worth” the effort of adding opioids to their regimens."
Summary of Main Points:
- The distinction of cancer vs non-cancer pain is made in opioid prescribing guidelines.
- PROP requested changes in opioid labels that made this distinction.
- FDA denied much of PROP's requests.
- The concept of cancer vs non-cancer pain has only been around in medical literature for a few decades.
- There isn't scientific evidence showing a clear distinction of how cancer vs. non-cancer pain is felt in the body.
- Many doctors and organizations have expressed concern with the cancer vs. non-cancer pain distinction.
- Some doctors and hospital systems are pushing for opioid-free cancer pain treatment.
- There is stigma involved in using opioids for cancer pain.
- Studies show that giving opioids to some terminal cancer pain patients may increase survival rate.
This content was written by Bev Schechtman and Carrie Judy for The Doctor Patient Forum. Updated February 7, 2022








