LIE: "The concepts of MME and MME limits are based on solid scientific evidence, and lowering patients to less than 90 MME is always beneficial."
The article contains the following information:
- What is MME?
- What is the purpose of MME conversions?
- Where did the MME conversions originate?
- What are some limitations of MME conversions?
- What is the origin of 90 MME and other MME thresholds?
- Do the CDC Guidelines use MME thresholds?
- Do data analytics use MME thresholds?
- Does lowering MME decrease adverse events like addiction or misuse?
- Does lowering MME reduce risk of overdose?
- Do forced tapers of high dose opioid" patients lower the risk of adverse events or death?
- Did CDC's updated/expanded guidelines use MME thresholds?
What is MME?
MME means Milligram of Morphine Equivalent, the amount of milligrams of morphine an opioid dose is equal to when prescribed." Why does it affect pain patients? "MME's are increasingly being used to indicate abuse and overdose potential and to set thresholds for prescribing and dispensing of opioid analgesics."
On June 7-8, 2021 the FDA held a workshop discussing MME. They discussed in depth the benefits of MME, the limitations of MME, how the calculations are done, etc. Much of the information you'll read here is from that workshop. There is a recording of both days (June 7 and June 8), in case you're interested in listening. Here is the link to all of the information from the presentations, including pdf documents and comment periods.
The purpose of the FDA meeting was "to bring stakeholders together to discuss the scientific basis of morphine milligram equivalents (MMEs), which are widely used as metrics in multiple areas throughout the healthcare system." We will add some information to their points to show the origin of MME thresholds and how they are being applied and enforced. In summary, this article will discuss the benefits and limitations of MME, if there is a standard way to calculate MME, what thresholds they use, where the first threshold came from, how these thresholds are being enforced, and how all of it is affecting people in pain. I'll link sources to each point. Ok, here we go.
What is the Purpose of MME Conversions?
The original purpose of the MME conversion (taken from FDA presentation from Grace Chai, PharmD) was to assist clinicians in determining initial dose when converting an individual patient’s opioid therapy. The conversion factors were based on a small clinical study done in limited populations.
Where Did the MME Conversions Originate?
In the FDA presentation by Mary Lynn McPherson, she explains that “The conversion factors were based on information from multiple sources. After reviewing published conversion factors, consensus was reached among two physicians with clinical experience in pain management and a pharmacist pharmacoepidemiologist.” Here is the publication by Von Korff she's referring to. Von Korff is also a member of PROP
What Are Some Limitations of MME Conversions?
Calculations
Is there truly a standardized way to calculate MME? Not really. Dr. Dasgupta presented this information at the FDA meeting. His talk was called "Inches, Centimeters, and Yards: Overlooked Definition Choices Inhibit Interpretation of Morphine Equivalence." In this discussion, he explains there are actually four different ways to calculate MME based on different definitions used. The results are quite varied. Dr. Dasgupta presented a study to prove this point using the 4 different definitions of MME to calculate dosages of patients. He used the 90 MME threshold as "high dose" since that is a commonly enforced amount. The results illustrate that the method of calculations produced different MME amounts. So, the same patients who were considered "high dose" patients with one calculation method was not with the other. If you're interested in learning all the factors that go into the different methods of calculations, please listen to Dr. Dasgupta's presentation. He shows the limitations of each method and explains which method the CDC uses. You can find a conversion calculator on the CDC app. Read what they have to say about the importance of MME.
Listen to a new podcast where Dr. Joshi and Daily Remedy interviewed Dr. Dasgupta.
Pharmacogenetic variability, drug interactions and other limitations of MME
In Dr. Fudin's FDA presentation called "Individual Patient & Medication Factors that Invalidate Morphine Milligram Equivalents," he discusses limitations of MME including pharmacogenetic variability. In Dr. Fudin's paper called "The MEDD myth: the impact of pseudoscience on pain research and prescribing-guideline development." he explains limitations of MME conversions including pharmacogenetic variability and drug interactions. Referring to the limitations, Fudin states "these include patient-specific attributes, such as pharmacogenetics, organ dysfunction, overall pain control, drug tolerance, drug–drug interactions, drug–food interactions, patient age, and body surface area. The bottom line is that as the scientific concepts upon which prescribing guideline authors depend are flawed and invalid, so are the guidelines themselves. As a result, we posit that these guidelines are disingenuous and highly unethical...just as prescribing guidelines are based on flawed formulas and evidence, invalid concepts can make research invalid. We are thus compelled to consider whether outcome research that continues to rely upon the concept of MME is also invalidated by such. Our hope as researchers is that our colleagues will acknowledge this imbroglio and convert their processes of outcome research in a manner that will produce more valid and meaningful results for individual patients, rather than meaningless cohorts."
What is the Origin of 90 MME and Other MME Thresholds?
Now that we know that there isn't a standardized way to calculate MME, let's look at some of ways MME thresholds are codified into policies and even laws. Actually, before we list those, you may be wondering where the 90 MME threshold even came from. Since it's made into laws, many people might assume this threshold must be based on solid scientific evidence. Yet, that's far from the truth. So before we go into how these thresholds are enforced, let's look at where limits such as 90 MME come from. Years before the 2016 CDC Guidelines came out, a group of doctors got together in Washington state to write opioid prescribing guidelines. Not surprisingly, many of the same doctors who went on the form PROP and help with the creation of the CDC Guidelines, were in the group who wrote the Washington Guidelines. In an article about these guidelines, Dr. David Tauben was interviewed. He was one of the authors of the Washington Guidelines. When asked about the CDC Guidelines, Tauben said “there is not a single thing in the CDC guidelines that we don’t cover in more detail in the Washington Guidelines." The article goes on the explain that Tauben was the first person to come up with the idea of an MME threshold. His idea was a patient should be given no more than 120 mg of a morphine equivalent. "Based on his clinical experience, patients needing more than 80 mg equivalent often did worse, not better. By 2006, at least 10,000 people in state insurance plans were prescribed more than 120 mg a day so the group set 120 mg as a first, more practical top dose limit before the patient should consult a pain specialist." So this was an idea pulled out of thin air based on one doctor's opinion, not solid scientific evidence. The CDC lowered that dose from 120 MME to 90 MME.
Dr. Gary Franklin, another PROP doctor who was involved with writing these guidelines, discussed the origin of the MME threshold in this lecture he gave in 2016.
Franklin said "Washington state did the first guideline in the US with a dosing threshold. We didn't have any clear cut data on what the dosing threshold should be and we came up with 120 MME, we thought it was a reasonable guess because in their experience they didn't think people needed much more than that. If fact, it started out at 90 but there were so many people in the state over 100 that they didn't think it was a practical threshold so we went up to 120 and that was what was implemented."
So the first MME threshold was 120 MME created by Dr. Tauben for the 2007 Washington guidelines. We know the CDC Guidelines came out in 2016. What happened between 2007 and 2016? On July 25, 2012, the anti-opioid zealots in the organization PROP submitted a citizen's petition to the FDA. Here is a pdf copy of the petition. Among the requests of changes to opioid analgesic labels, PROP asked the FDA to "add a maximum daily dose, equivalent to 100 milligrams of morphine for non-cancer pain." The FDA responded to PROP in 2013. A copy of their response is here.. Although they did grant some of PROP's requests, The FDA did not agree with their points regarding 100 MME threshold. We've listed a few quotes from their response to PROP:
- "The Agency declines to specify or recommend a maximum daily dose or duration of use for any opioid at this time."
- "Many professional societies did not support the Petition and stated that the data cited by PROP did not support PROP's requests (particularly those requests for limits on dose and duration of use of opioids)"
- "Professional societies also expressed concern that the labeling changes requested by PROP were not supported by scientific evidence, and that a "one-size-fits-all" approach to a maximum dose or duration of treatment would be problematic and inconsistent with the need for individualized treatment and the variability among patient responses to opioids."
- "The Agency declines to specify or recommend a maximum daily dose or duration of use for any opioid at this time."
- "FDA acknowledges that the available data do suggest a relationship between increasing opioid dose and risk of certain adverse events. However, the available information does not demonstrate that the relationship is necessarily a causal one."
- "The scientific literature does not support establishing a maximum recommended daily dose of 100 MME."
Do the CDC Guidelines Use MME thresholds?
After the FDA denied some of PROP's requests for regulating opioids, another agency took on the task of creating guidelines for opioid prescribing. This produced CDC's 2016 guidelines for opioid prescribing. Recommendation #5 of the Guidelines is the following: "When opioids are started, clinicians should prescribe the lowest effective dosage. Clinicians should use caution when prescribing opioids at any dosage, should carefully reassess evidence of individual benefits and risks when increasing dosage to ≥50 morphine milligram equivalents (MME)/day, and should avoid increasing dosage to ≥90 MME/day or carefully justify a decision to titrate dosage to >90 MME/day."
When the Opioid Workgroup (OWG) at the CDC met to discuss each proposed guideline, some members had concerns about this specific recommendation. The report (pdf) included the following comment: "One member of the Workgroup strongly opposes Guideline Recommendation #5 as it is written. This member stated repeatedly that the current recommendation clearly suggesting dose limits is not supported by any data showing a decrease in benefit/risk ratio at the arbitrary numbers stated in the recommendation. This member expresses concern that the current wording of Guideline Recommendation #5 will undermine support for the entire Guidelines from providers and professional organizations."
In order to assist in implementing the CDC Guidelines, the CDC BSC (Board of Scientific Counselors) discussed their plan to track and ensure they are being used. They discussed a plan to do this at the BSC meeting on September 7, 2016. Their plan was called The Quality Improvement (QI) Initiative. Their meeting notes stated that their plan "begins with creating QI measures that are tied or connected to the recommendation statements in the Guideline. A draft has been created of those measures, and NCIPC will work with a contractor (Abt Assoc.) to reach out to a broader group of stakeholders to test whether the measures are feasible and accurate, and whether health systems will have data available through an EHR to make tracking adjustments. It is not enough to have measures; it is important for health systems to implement the measures in their practice. To that end, NCIPC is developing an Implementation Guide document with support materials to help a health system implement the QI measures." The is stated in the section of the implementation guide that discusses specific MME thresholds. "Research has found that patients who receive high MME dosages have significantly increased risks of overdose compared with patients receiving low dosages. Establishing a practice wide policy on dosage levels may assist prescribers in making evidence-based decisions and minimizing risks of adverse outcomes. Use extra precautions when increasing to ≥ 50 MME per day, such as: Avoid or carefully justify increasing dosage to ≥ 90 MME per day. Patients already at high levels may be willing to try reducing the dosage. The practice should consider advising prescribers, as a matter of policy, to discuss this with their patients who are taking more than 50 MME per day."
Another part of CDC's implementation plan was with CDS (Clinical Decision Support), which not surprisingly AHRQ was involved with. Their BSC notes stated "Another area, Clinical Decision Supports, links the content of the Guideline to EHRs. If EHRs are an important part of clinical care, it is important that they include codes, artifacts, and alerts that are tied to, for instance, MME thresholds."
Do Data Analytics Use MME thresholds?
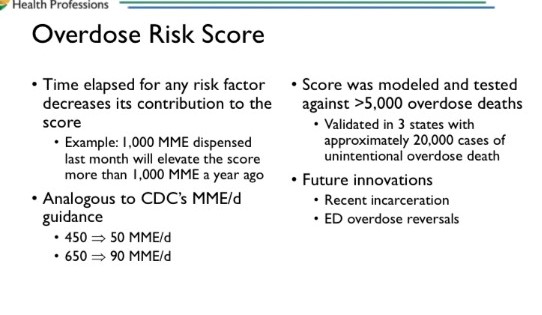
Unfortunately, CDC's implementation guide and Clinical Decision Support tools weren't the only places these MME thresholds were measured. Data Analytics companies created AI (Artificial Intelligence) risk scores that used MME thresholds as one of their main measures. NarxCare is one of these risk score algorithms. (Read our article about NarxCare here) As we've discussed, NarxCare is software owned by Bamboo Health. It pulls information from different data sources to spit out a risk score between 0-999. Since the algorithm is proprietary, we don't know exactly what they use, but we know some of the data points that are considered "red flags." One data point is MME. In their user guides, Bamboo Health explains that only 1% of all patients will have a risk score of 650-999. As shown in the following image from their user manual in Virginia if a patient gets 90 MME or higher, the patient's risk score is automatically 650+, which is the top 1% of all patients. Bamboo Health also has a similar scoring system of doctors.
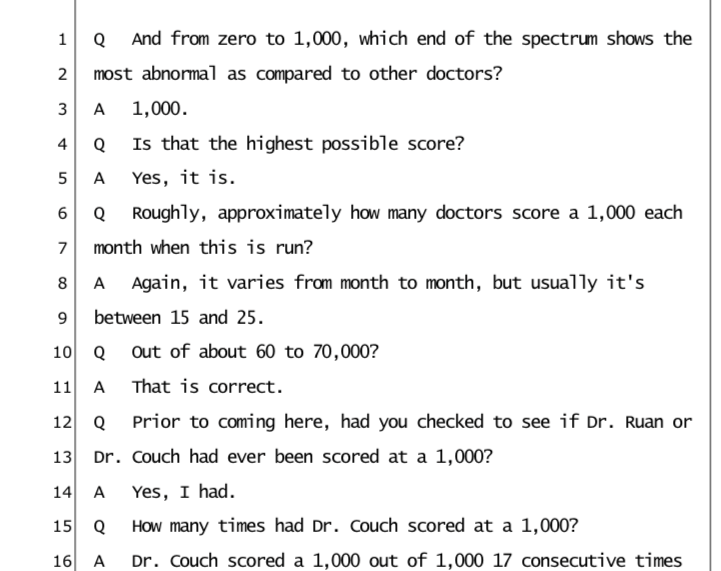
NarxCare isn't the only algorithm that uses MME to give risk scores. OIG (Office of Inspector General) contracts out with a company (Qlarant) that uses an algorithm to give doctors risk scores. This score is also 0-1000. Here is the OIG Toolkit, if you're interested in reading more about this scoring system. The site explains that "These toolkits provide steps to calculate patients' average daily morphine equivalent dose (MED/), which converts various prescription opioids and strengths into one standard value. This measure is also called morphine milligram equivalent (MME)." We know that this risk score was used in cases against doctors. The case that's going to be heard before the Supreme Court on March 1, 2022 involving Dr. Couch, used a risk score to target him. Here is our article about this Supreme Court case. Here is an image from Dr. Couch's court transcript where it shows Dr. Couch had a risk score of 1000 out of 1000.
Unfortunately, even though CDC has repeatedly said that the guidelines were just guidelines and shouldn't be used as law by enforcing MME limits or duration of prescription, as Dr. Dasgupta stated in his presentation , MME per day thresholds are "enshrined in state laws, with the assumption that it is a standardized metric." At the time of his presentation in June there were 14 states that had laws based on MME that imposed limits on the dosage of opioids that can be prescribed, ranging from 30 MME to a 120 MME. Here is a complete list of state laws regarding opioids.
As we've shown, these MME thresholds are used to create risk scores for patients and for doctors. We've seen several press releases put out by the DEA mentioning that the doctor they targeted "prescribed outside of the recommendations of the CDC Guidelines," including mentioning MME thresholds. So is it just a suggested threshold? How can it be when laws are created, patients are targeted, and doctors are arrested based on these arbitrary MME thresholds. As we have shown in this article, not only is the way to calculate MME not uniform or scientific, the very idea of an MME threshold was created by the opinion of doctors and not on solid scientific evidence.
Does Lowering MME Decrease Adverse Events Like addiction or Misuse?
In Grace Chai's FDA presentation, she said "Studies have also examined the association between daily dose and adverse outcomes (e.g., opioid use disorder/addiction, misuse/abuse), but causality is unclear."
Does Lowering MME Decrease Risk of Overdose?
A comment given by Friedhelm Sandbrink, who works for the VA: "We also know that in regard to overdoses in veterans, that the role of the actual prescription and the dosage and duration, while linked to higher risk, is actually relatively minor compared to the risk associated with comorbidities of the individual patient. When we look at high dose opioid prescribing, patients that are on more than 90 MME - those patients represent only 20% of the patients that overdosed from opioids or had a suicide related to being on opioids. While we know that the dosage is a factor, a history of having PTSD or Alcohol Use Disorder is just as strong as a factor of being on 120 MME. Opioid/benzo affects overdose rate by 1.4 where as depression affects it by 5. We have to get away from concentrating on the prescription and truly look at the patient. We have to see this as a whole person perspective. Train our providers in patient centered care. Taking the pain condition take into account with the comorbidities, in addition to looking at the pain prescription itself."
It is a factor, but not the only or even the most important factor. Using it as the sole factor to cause a patient to be red flagged or a doctor to be targeted isn't based on evidence. Dr. Stefan Kertesz said "If one can actually calculate dose- per Dasgupta- there is an association between the Rx dose and death risk but, this is like many situations in medicine where the overall risk to a patient is the net result of an array of risk factors, with dose prescribed being a modest one among many. " He also said "In most of medicine when we discuss risks we do so with reference to a collection of risk factors and the data we have permit that with Rx opioids too. It is simply a choice by CDC guideline authors not to use that data."
In a video Dr. Kertesz calls "Irrational Exuberance, Incautions Stoppage: Our Prescription Opioid Story" he reviews that even in VA data, most overdose among prescription recipients is at low prescribed dose. "This means that we are dealing with an event, an event that is driven by multiple factors, and specifically one that is probably best called 'a poisoning event with opioids involved' so that we avoid the incorrect inference that the written dose on the bottle is what causes it."
As far as the tremendous emphasis put on MME as an overdose factor, Dr. Kertesz said "We have so many scientific papers to show us that the actual risk of an overdose event is driven by a web of risk factors, just like the risk of any other medical event. It's frankly bizarre to choose precisely one risk factor and make a fetish of it the way we have with morphine milligram equivalents. It violates everything we know about opioid overdose, and it is entirely at odds with how medical professionals conceptualize all other risks we ordinarily consider. I can only speculate as to why we should take such a bizarre approach in regard to opioids. But in all likelihood it reflects the poor quality of our own training in both pain and addiction, and the powerful desire of regulators to reduce opioid questions down to something they can digest quickly, preferably between appetizers and the first course of a 5 course meal."
Do Forced Tapers of "High Dose Opioid" Patients Lower the Risk of Adverse Events or Death?
After the release of the 2016 CDC Guidelines, many pain patients across the country have been forced off of their opioid medications. Some forced off completely, and some forced to taper down to 90 MME. It happened so often that the FDA released a warning about not forcing rapid tapers and the CDC released a warning about misapplication of their guidelines. Neither document helped the situation, though. Rapid and forced tapers continue to occur daily.
One reason doctors are forcing patients off of opioids or down to 90 MME is because they are afraid to be targeted by the DEA. They have every reason to be worried, as we've proven in this article. DOJ is using MME thresholds to target targets. Another reason that doctors give for force tapering patients is they say it decreases risk of adverse events or overdoses. Is this actually backed by science, though? No, it's not. Read all about it in this study that was released showing that forcing tapers of patients who were on "high doses" of opioids causes more deaths than allowing them to remain on their medication. This decline in opioid prescribing has even affected cancer and hospice patients, as shown in this article. "In response to the opioid epidemic, the study authors suggested, measures to make opioids harder to obtain may have prevented some patients from receiving appropriate prescriptions for opioids to manage cancer pain."
Did CDC's 2022 updated guidelines remove MME Thresholds?
The following was information about the updated CDC Guidelines when they were in draft form including discussions with the Opioid Work Group
As we've shown, MME thresholds aren't a good idea and using arbitrary cut-off MME limits have caused great harm. The CDC is releasing updated (expanded) opioid prescribing guidelines this year (2022). Three of the suggested guidelines include MME thresholds. We will list each suggested guideline along with comments of concern from the OWG (Opioid Workgroup) members. Here is the full OWG report.
Recommendation #4: When opioids are started for opioid-naïve patients with acute, subacute, or chronic pain, clinicians should prescribe the lowest effective dosage. If opioids are continued for subacute or chronic pain, clinicians should use caution when prescribing opioids at any dosage, should carefully reassess evidence of individual benefits and risks when considering increasing dosage to ≥50 morphine milligram equivalents (MME)/day, and should avoid increasing dosage to ≥90 MME/day or carefully justify a decision to titrate dosage to >90 MME/day.
Opioid Workgroup Comment for #4: Many workgroup members voiced concern about the dose thresholds written into the recommendation. Many were concerned that this recommendation would lead to forced tapers or other potentially harmful consequences. Though workgroup members recognized the need to have thresholds as benchmarks, many felt that including these thresholds in the supporting text could serve to de-emphasize them as absolute thresholds, and thus recommended removing the specific MME range from the recommendation. In addition, these thresholds are felt to be arbitrary to some degree and could be calculated differently based on different conversion formulas, but when they appear in the statement, they appear to be authoritative.
Recommendation #5: For patients already receiving higher opioid dosages (e.g., >90 MME/day), clinicians should carefully weigh benefits and risks and exercise care when reducing or continuing opioid dosage. If benefits do not outweigh harms of continued opioid therapy, clinicians should optimize other therapies and work with patients to taper opioids to lower dosages or to taper and discontinue opioids.
Opioid Workgroup Comment for #5:
- 1. Similar to the observations noted for recommendation #4, many workgroup members felt that the threshold doseshould be removed from the statement and included in the supporting text.
- 2. Several workgroup members noted that the framing of this recommendation is not balanced – that it does not include the risk/benefit calculation of continuing opioids. For example, a more balanced approach is to have one sentence about continuing opioids and one sentence about tapering opioids in terms of risk/benefit analyses.
- 3. Some workgroup members felt more discussion is needed regarding working with patients or obtaining consent from patients when prior to initiating and prior to tapering opioids, and limiting involuntary tapering.
- 4. However, there were some specific issues that were noted as concerning by some members, these included: never going back up in dosage during opioid tapering; lack of inclusion of observational studies showing potential dangers of tapering; minimal discussion about risk of tapering; role of patient-centeredness approach; representing the role of buprenorphine as established rather than emerging; an explicit discussion of goals of tapers is needed, particularly related to public health versus individual patient outcomes; there seems to be an underlying assumption that the goal is to get to zero MME, but perhaps it should be to get to a safer dose or better symptoms or function; a section on iatrogenic harms of tapering may be warranted.
Recommendation Statement #8: Before starting and periodically during continuation of opioid therapy, clinicians should evaluate risk for opioid-related harms and discuss with patients. Clinicians should incorporate into the management plan strategies to mitigate risk, including offering naloxone when factors that increase risk for opioid overdose, such as history of overdose, history of substance use disorder, higher opioid dosages (≥50 MME/day), or concurrent benzodiazepine use, are present.
Opioid Workgroup Comment for #8: In addition, specifying the 50 MME dose threshold is concerning, and conveys similar risk as the other conditions. The dose threshold is arbitrary and inconsistent with other sections of the guideline (50 vs. 90 MME). As noted in overarching themes, many members recommended that these specific conditions be removed from the recommendation.
Will the CDC BSC take these comments into account when publishing the final expanded CDC Guidelines for opioid prescribing? We can only hope. Here is our Newsletter that explained all about the updated/expanded upcoming CDC Guidelines. Considering they didn't take into account the concerns from the OWG for the 2016 CDC Guidelines, it's doubtful they will this time around. Read our article explaining the way the 2016 Guidelines were written and how there was bias and lack of transparency.
The following is information about the published 2022 CDC Guidelines
Although the CDC repeatedly told media it loosened the updated guidelines by removing MME thresholds, it hasn't helped at all. In fact, all the did was remove the MME thresholds from the main bullet points, but they actually made them appear more strict throughout the document itself. In the 2016 guidelines, CDC mentioned 50 MME 18 times. In the 2022 guidelines, they mentioned 50 MME 23 times. We've had quite a few pain patients tell us they've been forced down to 50 MME due to the updated CDC guidelines. While CDC's Christopher Jones has claimed the updated guidelines removed these thresholds, PROP members such as Dr. Jane Ballantyne shed a different light on the update.
Listen to Dr. Ballantyne discuss this topic in a recent webinar in April 2023:
Dr. Dasgupta quotes a chronic pain representative named Liz Joniak-Grant “It is disheartening, but unfortunately not surprising. Far too often, we are victims of the good intentions of those wanting to ‘do something’ about the opioid overdose epidemic, but the something that is done oversimplifies the problem and pushes cookbook medicine upon those of us with complicated medical situations. And while everyone debates whether the MME limit was the right thing to do, we are forced to live by it, because medical personnel and others treat guidelines as mandates. So we wait. And we suffer. And we hope it will all get sorted so we can get the care we need.”
You may be wondering if the FDA has plans to do something with the MME information from their workshop. Dr. Chad Kollas, a palliative care doctor who is also on the AMA Opioid Task Force, e-mailed the FDA to ask that very question. With his permission, we are posting this e-mail thread for you.
From Dr. Kollas to the FDA : "I am reaching out to ask whether the FDA made any sort of summary document or recommendations based on the input from its Workshop on Morphine Milligram Equivalents. Frankly, I don’t even know whether creating a summary document was one of the goals of the Workshop, but I am very interested in any sort of FDA decisions or recommendations that might have arisen out of the session."
Response from FDA to Dr. Kollas: Thank you for your interest in the MME Workshop and reaching out to us on this. I have checked with the rest of the team and as you guessed, as of right now, we do not have anything additional such as a summary of the workshop, etc., so outside of what is already publicly available on our workshop webpage (Morphine Milligram Equivalents: Current Applications and Knowledge Gaps, Research Opportunities, and Future Directions - 06/07/2021 - 06/08/2021 | FDA), I have nothing new to share. I note that the transcripts of the meeting have posted to that webpage, but they of course are not a summation. I will let you know that there was a huge amount of interest in this topic and we continued to receive submissions to the docket from many interested parties even after the meeting which now become part of the official record of the meeting. We continue to feel the topic is important and bears continued discussion and exploration, so we hope to be able to continue exploring and working on it, especially continuing to interact with our other federal and international partners that participated in the workshop, not to mention patient and professional groups. Again thank you for your interest, and feel free to continue to check back periodically to see if we have any new information we can share publicly on this topic."
In addition to the FDA workshop information, if you're still interested in learning more about MME, we also recommend this article by Josh Bloom. Dr. Bloom's comment for the FDA workshop also has great information.
https://www.acsh.org/news/2021/05/24/comments-fda-opioid-dosing-based-milligram-morphine-equivalents-unscientific-15561
This content was written by Bev Schechtman and Carrie Judy for The Doctor Patient Forum. Updated May 4, 2023.








