LIE: "Studies show that opioids make pain worse in a common condition called Opioid Induced Hyperalgesia (OIH)."
This article contains the following information:
- Defining Terms
- What is the origin of the idea of Opioid Induced Hyperalgesia (OIH)?
- OIH in acute pain patients
- OIH in rats
- OIH in patients on Suboxone or Methadone
- OIH in Chronic Pain Patients (CPP's)
- What do other studies or articles say about OIH?
- Do doctors claim that OIH is a proven common condition?
- Why do "experts" give misleading information about OIH?
- Accurate diagnosis of OIH in CPP's
- Doctors views of OIH
- FDA - updated label for opioids including OIH
- Summary
Have you ever heard a medical expert say "Not only do opioids not work for chronic pain, but they actually often makes pain worse"? Ever wonder if it's true?
After researching this phenomenon called Opioid Induced Hyperalgesia (OIH), the one thing that's abundantly clear is that nothing to do with OIH is abundantly clear. Some doctors think it doesn't exist. Some think it is relatively common. Some think it is simply a conflation of terms. The definition isn't even agreed upon. Since the information on OIH is so conflicted, let's define some terms for the sake of this article.
Opioid Tolerance - Physiologic adaptation to the presence of an opioid in the body such that increased doses are required to maintain the same level of analgesia. When someone builds tolerance to opioids, increased doses are needed to achieve the same level of efficacy. The treatment for this is increased opioid dosage, decreased time between doses, or opioid rotation.
Opioid Withdrawal- Produced by abrupt cessation or rapid dose reduction. When a patient develops a physical dependence on opioids and feels pain when opioids are stopped or decreased. There are two phases of opioid withdrawal, an initial, acute phase and a second, chronic phase. Treatment is gradual reduction in opioid dosage.
Allodynia - Innocuous (non harmful) stimuli that is now painful, meaning something that is not normally painful at all becomes painful. An example of this would if the clothes you're wearing start causing pain just from touching your skin.
Central Sensitization - International Association of the Study of Pain (IASP) defines it as “increased responsiveness of nociceptive neurons in the CNS to their normal or subthreshold input." More simply it is when a patient becomes more and more sensitive to acute or chronic pain. This phenomenon was first discussed in the 1940's. An example of a condition with increased central sensitization is Fibromyalgia. This is similar/the same as hyperalgesia.
Hyperalgesia- Stimuli that is typically a little painful becomes extremely painful. An example of this is a small pin prick. In someone with hyperalgesia, the sensation of a small pin prick would be very painful. This phenomenon is basically the same as central sensitization.
Opioid Induced Hyperalgesia (OIH) - A paradoxical response: administration of opioids for the treatment of pain that actually causes higher pain sensitivity. A state of nociceptive sensitization (pain) caused by exposure to opioids. The idea of OIH is when a patient takes opioids, pain increases. This is different from tolerance, bc in OIH as the dose increases, so does the pain. Treatment is to reduce opioid dose or possibly rotate opioids.
Quantitative Sensory Testing (QST) - A variety of tests used to measure pain response to different stimuli. As long as a test can be quantified or measured, it can be used as QST. Some common QST's are thermal testing (both hot and cold), and pinprick test in humans, and a paw test in animals.
What Is the Origin Of the Idea Of Opioid Induced Hyperalgesia?
Many articles say that the idea of OIH was noted as early as 1870. It was recognized that a potent analgesic such as morphine could actually result in an increase in pain. In 1870 Dr.Albutt said “Does morphia tend to encourage the very pain it pretends to relieve?"
According to an Israeli expert, Erica Suzan, the phenomenon of OIH has been studied in the following groups for over 30 years:
- Healthy volunteers following acute opioid exposure
- Acute postoperative pain
- Chronic nonmalignant pain
- Cancer pain-end of life
- People addicted to opioids
The concept of Opioid Induced Hyperalgesia in acute postoperative settings is discussed in this presentation given at a meeting of International Association of the Study of Pain. Erica Suzan makes the following points in her lecture:
- Three conditions seem very much alike: acute withdrawal, acute tolerance, acute OIH. Although they seem alike they are very different in terms of treatment.
- In true OIH in acute as soon as opioids are given, pain increases.
- In her opinion even though many of the findings of studies claim they prove OIH exists in post-op patients, those studies measure acute opioid withdrawal as opposed to true acute OIH.
- "True clinical OIH is quite rare, and is seen mainly in cancer pain patients who receive mega doses of opioids usually at the end of life."
- Dr. Suzan suggests the following clinical criteria for diagnosing OIH:
- Increased pain intensity during ongoing opioid treatment
- No evidence for underlying disease progression
- No evidence for clinical or pharmacological opioid withdrawal
- No evidence of opioid tolerance
- Decrease in pain intensity in response to opioid dose reduction
- No evidence for addictive behavior
Opioid Induced Hyperalgesia In Rats
When people claim that studies show OIH is common, they are referring to a 1994 study published in The Journal of Neuroscience done on rats by Dr. Mao. This study clearly shows that OIH exists in rats. In this presentation by Dr.Jianren Mao, "Mechanisms of Opioid-induced Hyperalgesia," he claims that OIH exists in humans, although he acknowledges that studies don't yet back up that claim. Here are some points:
- The concept of OIH was introduced in 1994 in his study in a lab with rats.
- He included the following slide showing results from this study:
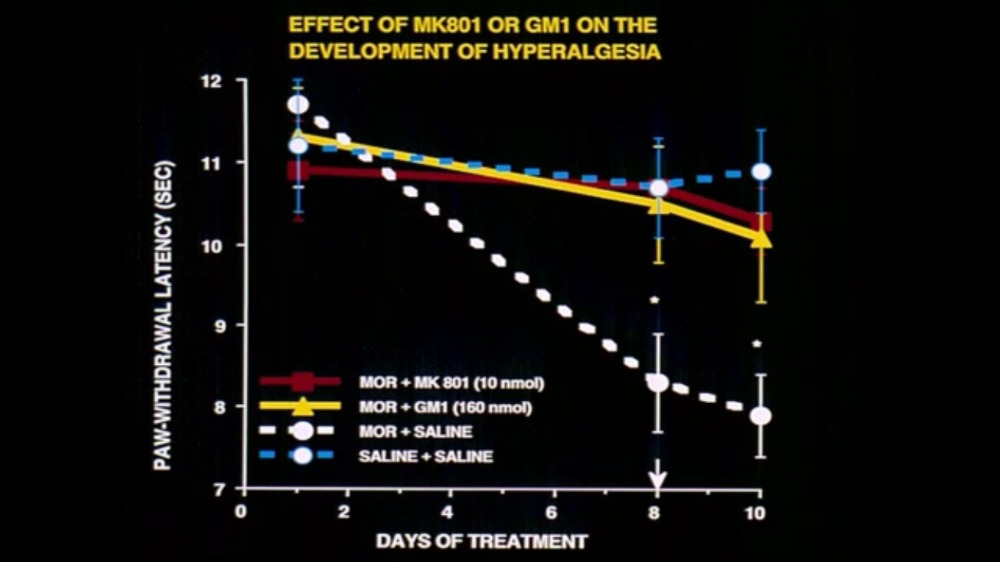
- Rats were treated with morphine vs. saline and they performed QST's (Quantitative Sensory Tests).
- The purpose of the study was to test tolerance; he calls the results of OIH a serendipitous finding.
- He claims it was a significant finding in the laboratory but didn't make its way into the clinical area until the early 2000's.
- He speculates possible explanations of OIH.
- "After 25 years we still don't have a tool in a clinical setting to differentiate between opioid tolerance and OIH."
After listening to Dr. Suzman's presentation, I asked an ER doctor if he had ever seen the phenomenon of OIH in acute pain patients. His response was "I've never had a hospice patient react that way, and I've cared for many people at the end of life. While I wouldn't rule out some incredibly rare paradoxical reaction, I suspect the truth is much simpler: sometimes you give people pain medicine while their pain is getting worse and it's better than it would have been otherwise, but still more than it was the last time you assessed it...anything's possible, but I've never seen that happen."
OIH In Patients On Methadone or Suboxone:
If OIH exists in pain patients, it would be logical for it to exist in patients with OUD. There have been many studies about this. Some have concluded that OIH does exist in OUD patients on opioid therapy. After reading many of them, it seems like it's impossible to tell if the patient was experiencing true OIH or if the patient just had built a tolerance to opioids. A study called Buprenorphine Maintenance Subjects are Hyperalgesic and Have No Antinociceptive Response to a Very High Morphine Dose concluded "buprenorphine subjects, compared with controls, were hyperalgesic, did not experience antinociception (pain relief), despite high morphine concentrations." Remembering the criteria Dr. Suzan discussed for diagnosing true OIH, I would say this study didn't differentiate between tolerance and OIH. Pain didn't worsen with opioids, but pain relief was not achieved with high doses.
Here is a quote from an article "This relative pain intolerance has been ascribed to the phenomenon of opioid-induced hyperalgesia. Unfortunately, a causal role for opioids in producing hyperalgesia has yet to be conclusively demonstrated in patients, both those receiving opioids for the treatment of addiction or chronic pain. The data reflecting hyperalgesia in opioid-dependent patients at this time are cross-sectional only, comparing opioid-dependent and opioid-free samples, but not comparing the same individuals before and after opioid administration. For compelling clinical and ethical reasons, it is near impossible to design such a pre-post study, leaving open the question of whether the hyperalgesia suffered by methadone and buprenorphine patients is, in fact, opioid-induced."
I spoke to two Harm Reduction experts to see if they've seen OIH in patients on methadone or Suboxone. Both said they've never seen anyone experience this.That doesn't prove it doesn't exist, but if it does, it seems to be exceedingly rare.
Opioid Induced Hyperalgesia in Chronic Pain Patients (CPP's):
Dr. Norman Harden, a doctor known for his work in CRPS (Complex Regional Pain Syndrome), gave a presentation at Painweek in 2016 called "Opioid 'Induced' Hyperalgesia and Allodynia: The description of the lesson was "Prolonged exposure to opioids hypothetically activates a pro-nociceptive mechanism resulting in opioid induced hyperalgesia (OIH). Opioid hysteria doctors are causing payors and governing bodies to rush to bring the OIH concept into law and protocol, but are finding a lack of any scientific evidence for this process, at least in humans. The FDA is now requiring pharma to run extensive and expensive trials to demonstrate OIH associated with opioid therapy, but the construct is vaguely defined, the mechanisms are poorly understood, and the outcomes and methods for studying OIH are very poorly developed."
Here is a short synopsis of this presentation from Dr. Harden.
A few years before this Pain Week presentation, Dr. Harden gave a similar presentation at a 2015 AAPM (American Academy of Pain Medicine) annual meeting. This article in Medscape called "Complexities of Opioid-Induced Hyperalgesia Poorly Understood," is an excellent summary and explanation of his talk.
- "Opioid-induced hyperalgesia is among the most pressing concerns in the national discussion of opioid addiction, underscored by the US Food and Drug Administration's (FDA) call for clinical trials to better understand the risks."
- There is very little agreement and a lot of confusion surrounding the idea of Opioid Induced Hyperalgesia (OIH).
- Studies are clear that OIH exists in rats, and many have made the assumption that it also works the same way in humans. Yet, there is limited data backing up this claim.
- The confusion is due to frequent conflation with tolerance, Hyperalgesia/Allodynia-which is central sensitization that can normally be found in chronic pain patients, and true OIH. (See definitions above),
- In order to better understand OIH and the frequency of it , Dr. Harden and his colleagues conducted a study that was supported by Northwestern Memorial Hospital. It compared pain test responses among patients with chronic low back pain. The following is a break down of the study:
- 10 patients were receiving opioids and 10 were not.
- "The results showed no significant differences between the groups in terms of sensory tests for pain."
- Of all the tests only one test showed statistical significance, which actually showed a greater sensitivity in the non opioid group, so in this Quantitative Sensory Testing people on opioids had lower pain than the non opioid group.
- "The early findings appear to support the assertion that hyperalgesia (central sensitization) in many cases may be part of the natural progression of chronic pain."
- "It very difficult to demonstrate hyperalgesia in pain patients on opioids because you do not know what the hyperalgesia is from."
What Do Other Studies Or Articles Say About Opioid Induced Hyperalgesia?
The phenomenon of OIH has been studied and written about, but very little true evidence exists. As we said earlier, nothing about OIH is standard or agreed upon by medical experts or scientists. Let's look through some articles/studies that discuss OIH:
The background of this study: "Very little is known regarding the prevalence of opioid induced hyperalgesia (OIH) in day to day medical practice. The aim of this study was to evaluate the physician's perception of the prevalence of OIH within their practice, and to assess the level of physician's knowledge with respect to the identification and treatment of this problem."
Results of this study: "In this study, the suspected prevalence of OIH using the average number of patients treated per year with opioids was 0.002% per patient per physician practice year for acute pain, and 0.01% per patient per physician practice year for chronic pain."
The conclusion of this study: "The perceived prevalence of OIH in clinical practice is a relatively rare phenomenon. Furthermore, more than half of physicians did not use a clinical test to confirm the diagnosis of OIH. The two main treatment modalities used were NMDA antagonists (such as ketamine) and opioid rotation. The criteria for the diagnosis of OIH still need to be accurately defined."
Abstract of the study: Although often successful in acute settings, long-term use of opioid pain medications may be accompanied by waning levels of analgesic response not readily attributable to advancing underlying disease, necessitating dose escalation to attain pain relief. Analgesic tolerance, and more recently opioid-induced hyperalgesia, have been invoked to explain such declines in opioid effectiveness over time because both phenomena result in inadequate analgesia."
Key point: "It is not possible to distinguish between tolerance and opioid-induced hyperalgesia solely based on the clinical observation of the need for dose escalation. Furthermore, although treatment of opioid tolerance usually involves dose escalation, opioid-induced hyperalgesia is treated by dose reduction and initiating alternative analgesic strategies. The prevalence and relevance of these 2 distinct phenomenon or the efficacy of chronic opioid therapy for the treatment of chronic painful conditions remain inadequately investigated."
Results of the study: "After 1 month of oral morphine therapy, patients with chronic low back pain developed tolerance but not opioid-induced hyperalgesia. Improvements in pain and functionality were observed." Our study provides the first high-quality prospective evidence for the development of tolerance and absence of opioid-induced hyperalgesia after 1 month of chronic opioid therapy."
Conclusions of the study: "This study is not meant to discount the abundance of data from animals and case studies documenting isolated cases of severe opioid-induced hyperalgesia. Clinicians may still suspect expression of opioid-induced hyperalgesia when opioid treatment becomes entirely ineffective and pain becomes increased and widespread, even in the absence of disease progression."
Misuse of Hyperalgesia to Limit Care
In this article a doctor discusses the case of one of his patients who was a CPP diagnosed with stage IV lung cancer.
- His insurance company was concerned about the expenses of his medicine and asked the doctor to arrange a second opinion.
- "The report stated 'given his high doses, the patient is likely suffering from opiate-induced hyperalgesia and would actually benefit from weaning his daily opiate intake.'”
- The insurance company refused to pay for his medicines until the doctor gave them a report on his plan to take him off his medicines.
- The doctor stated :
- Fishbain et al did an evidence-based structured review of 504 articles on OIH in humans and animals. They addressed ten hypotheses that had been utilized to test for the possibility of OIH in humans. Only studies performed on opioid naïve, pain-free volunteers that were given opioid infusions met criteria for quality evidence—and even those studies showed inconsistent results."
- "I am afraid that our concern with the laboratory curiosity of OIH will end up feeding opiophobia and will be used as an excuse by clinicians to avoid the complexities of opioid analgesia or by insurance companies to limit access to care for “expensive” chronic pain patients. In our attempts to optimize therapy for chronic pain patients, we must be careful not to “throw out the baby with the bathwater.”
Do Opioids Induce Hyperalgesia in Humans? An Evidence-based Structured Review
- Published in 2009, a systematic review of other studies. These included 30 studies and 18 case reports or case series studies.
- "There was insufficient evidence to determine the existence of opioid-induced hyperalgesia in humans, except for normal volunteers receiving opioid infusions, but these data were inconsistent."
Opioid-induced hyperalgesia (OIH): a real clinical problem or just an experimental phenomenon?
- "Although opioid-induced hyperalgesia (OIH) is mentioned as a potential cause of opioid dose escalation without adequate analgesia, true evidence in support of this notion is relatively limited."
- "Thus far evidence for OIH in patients with chronic or cancer-related pain is lacking."
Do Doctors Claim That OIH is a Proven Common Condition?
Yes!! It seems like this has become a common talking point of people like Andrew Kolodny and other members of PROP. I'll list some examples:
New Opioid Guidelines - How Colorado Can Revolutionize Pain Management
A presentation was given by Dr. Don Stader, an ER doctor who owns a compliance company called Stader Opioid Consultants and has created an opioid free approach to ER medicine called ALTO (Alternatives for Opioids for Pain Management).
- Strangely enough, he gives a lecture on the danger of prescription opioids while drinking a beer.(We had linked to a video of his lecture, but he must have removed it from the internet).
"Here is the mind bending thing. Opioids cause chronic pain is what we're discovering." ~ Dr. Don Stader
Opioids - The Big Picture - Two doctors in Canada give a history and overview of opioids. They repeat all of the major lies/false narratives of Andrew Kolodny and PROP .
- "100 years ago Dr. Calkinis already knew that opioids cause pain."
- "When I teach and I talk to residents and medical students about the fact that opioids cause pain, they look at me like I have two heads, yet 150 years ago we already knew this."
- "We already know that it causes hyperalgesia."
The Psychological and Physical Effects of Pain Medications
This article is written by Dr. Don Teater for the National Safety Council (NSC).
- "Though the frequency of opioid-induced hyperalgesia is unknown, it is believed to be fairly common and significant.
Why Do "Experts" Give Misleading Information About Opioid Induced Hyperalgesia?
Insurance companies want to save money
An article, "Demystifying Opioid-Induced Hyperalgesia," discusses this point.
- "Some insurance companies have declined to continue paying for opioid medications, citing OIH."
- "In cases like these, many insurance companies state that patients should have their doses tapered in order to decrease their pain. However, clinicians may find that attempts to reduce the opioid dose often result in increased pain."
- "Despite these experimental studies, no published studies have either specifically evaluated the relevance of OIH to clinical populations of chronic pain patients or provided evidence that OIH actually contributes to increased opioid need in chronic pain patients."
- "There are several well-established reasons other than possible OIH to explain why prescribers often find it necessary to increase the opioid dose in a patient with chronic pain. If a patient is functioning with adequate pain relief on his/her current dose of opioid, decreasing the dose, as the insurance company may suggest, is not in the patient’s best interest. The outcome of such a decision is likely to be increased pain and decreased function."
Used as part of the litigation Narrative
We frequently refer to the litigation narrative. Most of the people who repeat common false narratives such as OIH are also paid expert legal witnesses in opioid litigation. Some of the repeat expert legal witnesses in litigation are Andrew Kolodny, Jane Ballantyne, and Anna Lembke. All three discuss OIH as if it were common and backed by science. The existence and prevalence of OIH can be found in most of the opioid litigation lawsuits. I'll list two of them:
Colorado vs. Purdue and Sacklers
- Page 24 "Although opioids may be effective for alleviating pain in the short-term, clinical studies indicate that opioids are not similarly effective for relieving chronic or long lasting pain. Patients are at risk of increased pain sensitivity (known as hyperalgesia) when using opioids for a prolonged period."
- Page 111 "At least one of L.S.’s patients suffered from “hyperalgesia from excessive opioids. L.S.’s medical license was revoked in October 2018."
A complaint filed against a doctor in NJ
- Page 11- "As explained by Lewis S. Nelson, M.D. opioids “have been increasingly documented to promote the development of ‘opioid-induced hyperalgesia.’” Dr. Nelson clarifies that these risks “are acceptable for the management of end-of-life cancer related pain, but are not acceptable for the management of a pain syndrome expected to last decades."
Doctors Are Afraid To Prescribe Opioids
I received hundreds of comments from CPP's on social media saying their doctors used OIH as a reason to deny opioids:
- "My doctor has used that as an excuse to cut my meds and force me off methadone. I haven’t experienced it. The only thing I experienced was plateauing on my dose after 20 years." ~CPP on Facebook
- "Supposedly the new pain management office I went to in 2013 diagnosed me with that. I had overuse injuries and herniated disc in my neck." ~CPP on Facebook
- "I was told that that was why my pain was so much worse OFF the drugs when I was cut. It was months later and they said it was still the aftereffects of the drug and that being on opiates MAKES ones pain worse so give it time." ~CPP on Facebook
- "I was told I don’t actually have the rare disease I've been diagnosed with and had major surgery for, I just have pain BECAUSE of opioids." ~CPP on Facebook
- "They tried saying they were tapering because of hyperalgesia." ~CPP on Facebook
- "Yep! My doctor swore my meds made my pain worse." ~CPP on Facebook
- "I was told that. I was taken off oxycodone 6 months ago. Pain is still there. It is not hyperalgesic pain. It is pain from a failed cervical spine surgery." ~CPP from Facebook
- "That was used on me to cut me off after my 35 years my retired." ~CPP on Twitter
Accurate Diagnoses of OIH in CPP's
I asked on the National Don't Punish Pain Facebook group (over 21,000 people) and on Twitter if any CPP's had experience actual OIH. I received a message from one pain patient saying she absolutely experienced OIH. She said it started after about one year on opioids.
Dr. Chad Kollas, a palliative care doctor who is also on the AMA Opioid Task Force:
His view of OIH: "OIH is very uncommon in our Clinic. I would feel very safe in saying that it affects less than 1% of our patients. I believe OIH is rare, but over-diagnosed by prescribers who are conflating it with other conditions (withdrawal in physical dependence, actual addiction, etc)."
How many patients has he seen with it?: Maybe 5 out of 40,000 patients "That said, critics will point out that a cancer center is not representative of the general population"
How did you treat your patients with OIH?: "When I have experienced patients with OIH, they have responded well to opioid rotation, especially to methadone."
Dr. Stefan Kertesz, a VA doctor who works with both pain patients and patients with addiction:
His view of OIH: "As I see it, the words "Opioid Induced Hyperalgesia" are now used to refer both to a narrow laboratory phenomenon that can be exhibited in animals and humans, and also generalized to refer to any and all situations where patients report worse pain while receiving opioids...I believe that it's possible for opioids to make pain more volatile. That's totally separate from the relatively uncommon phenomenon of "hyperalgesia."
Dr. Bob Twillman, a Pain Psychologist:
His view of OIH: "It's so hard to say definitively if it exists in an individual, and the only practical way to know is to taper them and see what happens. I'm not interested in that exercise unless there is a really good reason to think there's something there to be discovered. In no way do I think it's as common as the PROPagators think.-I've never seen a large-scale study proving that it's a 'thing' in humans, only rat studies."
FDA opioid label change to include OIH
In April 2023, the FDA announces a new label change for opioid medication.
The label changes are listed on the FDA's website and include:
- the risk of overdose increases as the dosage increases for all opioid pain medicines;
- IR opioids should not be used for an extended period of time unless a patient’s pain remains severe enough to require them and alternative treatment options continue to be inadequate;
- many acute pain conditions treated in the outpatient setting require no more than a few days of an opioid pain medicine; and
- it is recommended to reserve ER/LA opioid pain medicines for severe and persistent pain that requires an extended treatment period with a daily opioid pain medicine and for which alternative treatment options are inadequate.
The updates also include a warning about OIH for both IR and ER/LA opioid pain medicines, including information on differentiating OIH symptoms from those of opioid tolerance and withdrawal.
Here is a table listing the label changes.
On April 19, 2023, there was a meeting of the Anesthetic and Analgesic Drug Products Advisory Committee (AADPAC) The issue of OIH was discussed along with concerns about the design of possible studies.
- True Opioid Induced Hyperalgesia (OIH) is often conflated with other diagnoses such as tolerance and withdrawal.
- The idea of opioids causing pain was written about as early of 1870.
- The idea of OIH has been studied in the following groups:
- Healthy volunteers following acute opioid exposure
- Acute postoperative pain
- Chronic nonmalignant pain
- End of life pain
- People addicted to opioids
- The following criteria are needed for a true diagnosis of OIH:
- Increased pain intensity during ongoing opioid treatment
- No evidence of underlying disease progression
- No evidence of clinical or pharmacological opioid withdrawal
- No evidence of opioid tolerance
- Decrease pain intensity with opioid reduction
- No evidence of addictive behavior
- OIH has been proven in studies of rats, not people
- CPP's seem to have hyperalgesia that is unrelated to opioids.
- Many zealots say OIH is common and proven in studies.
- Insurance companies use OIH as a reason to deny coverage of opioids.
- OIH is cited in litigation.
- A diagnosis of OIH is often given to patients as a reason to not prescribe opioids.
- If OIH exists, it is exceedingly rare.
- More studies are needed to see if OIH is an actual phenomenon in people.
- FDA label change to include OIH 4/13/23
This content was written by Bev Schechtman and Carrie Judy for The Doctor Patient Forum Updated May 4, 2023








